 12 weeks NT scan photos - August 2018 Birth Club - BabyCenter ...
12 weeks NT scan photos - August 2018 Birth Club - BabyCenter ...A nuchal scan or translucent neck (NT) scan procedure / is a sonographic scan () to detect chromosomal abnormalities in, although altered composition of the extracellular matrix and limited lymphatic drainage can also be detected.
Since this may cause cardiovascular development, a translucent nuchal scan is used as a screening, rather than a diagnostic tool for such conditions, Edwards syndrome and Patau syndrome and non-genetic.
There are two different measurements: nuchal translucent size and thickness of the nuchal fold. Nuchal translucent size is typically assessed at the end of the first trimester, between 11 weeks 3 days and 13 weeks 6 days of gestation. Nuchal fold thickness is measured towards the end of the second trimester. As nuchal translucent size increases, the possibility of chromosomal abnormalities and increased mortality; 65% of the largest translucencies (> 6.5mm) is due to chromosomal abnormalities, whereas mortality was 19% in this size. Nuchal scan may also help confirm both the accuracy of the date of pregnancy and fetal survival.
All the women, whatever their age, have a small risk of having a baby with physical or cognitive disabilities. Nuchal scan helps doctors estimate the risk of a fetus having Down syndrome or other abnormalities are more accurate than the age of the mother alone.
Overall, most common chromosomal abnormality is Down syndrome (21). The risk increases with maternal age of 1 in 1400 pregnancies under the age of 25 to 1 in 350 at age 35, to 1 in 200 at age 40. Down syndrome is a chromosomal disorder second most common associated with increased nuchal translucent, after (45 , X). []
Until now, the only reliable way to determine whether the fetus has a chromosomal abnormality is to have such or, but these tests carry a risk of causing an estimated variously as a range between 1% [] or 0.06 %. Based on the age of the mother, some states offer an invasive test for women over 35; others to the oldest 5% of pregnant women. Most women, especially those who have a low risk of having a child with Down syndrome, may want to avoid the risk to the fetus and discomfort of invasive testing. In 2011, Sequenom announced the launch of MaterniT21, non-invasive blood test with a high degree of accuracy in detecting Down syndrome (and some other chromosomal abnormalities). In 2015, there were five commercial version of this screen (so-called cell-free fetal DNA screening) are available in the United States.
Blood tests are also used to look for abnormal levels or. The results of the three factors may indicate a higher risk. If this happens, women may be advised to have a screen that is more reliable as the cell-free fetal DNA examinations or invasive diagnostic tests (such as or).
Screening for Down's syndrome with a combination of age and fetal nuchal thickness translucent mother at 11-14 weeks of gestation was introduced in the 1990s. This method identifies approximately 75% of fetuses are exposed while screening about 5% of pregnancies. natural fetal loss after a positive diagnosis at 12 weeks is about 30%.
Other common chromosomal defect that causes thick, translucent nuchal
In fetuses with normal chromosome number, a thicker nuchal translucent associated with other fetal defects and genetic syndromes.
nuchal scan (NT procedure) is performed between 11 and 14 weeks of pregnancy, because accuracy is best in this period. scan obtained with the fetus and the fetal head neutral position (not hyperflexed or extended, both of which can affect the thickness of the nuchal translucent). Figure fetal enlarged to fill 75% of the screen, and the maximum thickness measured from the leading edge to the leading edge. It is important to distinguish the nuchal lucency of the underlying amniotic membrane.
normal thickness depends on (CRL) of the fetus. Among them are translucent fetal nuchal exceeds normal value, there is a relatively high risk of significant abnormalities.
An increased nuchal translucent increases the probability that the fetus will be affected by, or. Typically, nuchal translucent alone is not sufficient as a screening test for chromosomal abnormalities.
How to determine a measurement of nuchal translucent normal or abnormal can be difficult. The use of a single millimeter cutoff (such as 2.5 or 3.0 mm) is inappropriate due to the measurement of nuchal translucent usually increases with gestational age (around 15% to 20% per week of gestation 10-13 weeks). At 12 weeks gestation, the "average" nuchal thickness of 2.18mm was observed; However, up to 13% of normal fetal chromosomes comes with nuchal translucent greater than 2.5mm. Thus for greater accuracy of predicting risk, nuchal scan results can be combined with maternal blood test results simultaneously. In pregnancies affected by Down syndrome there is a tendency for the rate (hCG) increases and (PAPP-A) will decrease.
The advantage of a nuchal scan foregoing use only blood biochemical profiling notably a rate reduction.
nuchal scan only detects 62% of all Down syndrome () with a false positive rate of 5.0%; combined with a blood test gives the corresponding values of 73% and 4.7%.
In another study values of 79.6% and 2.7% for the combined screening is then increased by the addition of a second trimester ultrasound scan to 89.7% and 4.2% respectively. A further study reported the detection of 88% for trisomy 21 (Down syndrome) and 75% for (), with a false positive rate of 3.3%. Finally, using the additional ultrasound features of absent nasal bone can further increase the detection rate for Down syndrome for more than 95%.
When the screening is positive, (CVS) or testing is required to confirm the presence of a genetic disorder. However, these procedures carry a small risk of miscarriage so previous screening with low false positive rate is required to minimize the chances of miscarriage.
actual anatomical structure which is viewed as a translucent liquid normal possibility in the back of the neck, which can either be edematous or in some cases with lymphatic sac containing fluid widened in connection normal embryological change.
The area measured translucent (see-through nuchal) is only useful for measuring between 11 and 14 weeks of pregnancy, when the fetus is developing and high peripheral resistance. After 14 weeks of the lymphatic system may have developed enough to drain away any excess liquid, and changes in placental circulation will result in a decrease in peripheral resistance. So after this time any disorder that causes fluid accumulation may seem to repair themselves and thus go undetected by scanning neck.
The buildup in the liquid is due to a blockage of fluid in the fetus develops. wide-area progressive increase breaks during the measurement period 11- 14 weeks thus showing.
nuchal translucent testing distinctly different from and not to be confused with the nuchal thickness testing. At the end of the second trimester (26 weeks), translucent nuchal can no longer be seen and vice versa nuchal fold thickness was measured between 16 and 24 weeks gestation. fold more focused and at the level of the posterior fossa. These measurements have a higher threshold than normal, despite the implications of increased thickness similar to translucent. Nuchal fold thickness is considered normal if it is below 5mm between 16 and 18 weeks gestation and below 6mm between 18 and 24 weeks of pregnancy. Increasing the thickness corresponds to an increased risk for fetal abnormalities and others.
nuchal scan first came into widespread use in 2003.
 Nuchal scan - Wikipedia
Nuchal scan - Wikipedia High Risk 12 Week NT Scan - February 2017 - BabyCenter Australia
High Risk 12 Week NT Scan - February 2017 - BabyCenter Australia 12 Weeks: NT Scan | Between Two Evils
12 Weeks: NT Scan | Between Two Evils 12 Week Scan - Nuchal Translucency Scan
12 Week Scan - Nuchal Translucency Scan 12-13 Week NT Scan Ultrasound Video - YouTube
12-13 Week NT Scan Ultrasound Video - YouTube Nuchal Translucency Scan (11 Weeks - 14 Weeks) - YouTube
Nuchal Translucency Scan (11 Weeks - 14 Weeks) - YouTube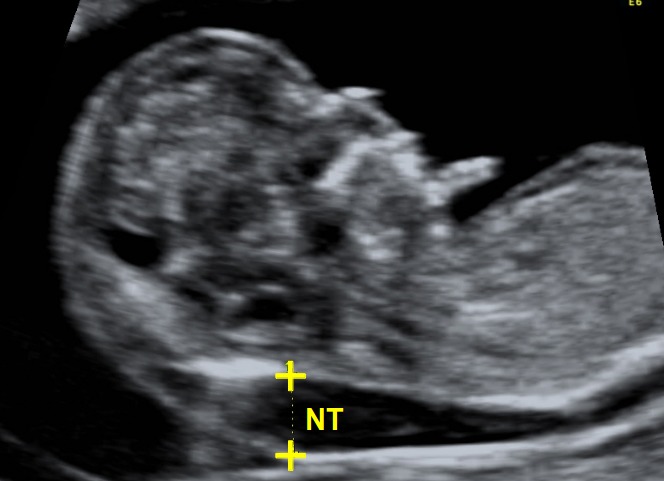 Nuchal translucency scan | Certificates of competence | FMF ...
Nuchal translucency scan | Certificates of competence | FMF ... 12 week NT scan, with a 95% gender guess! - September 2019 Birth ...
12 week NT scan, with a 95% gender guess! - September 2019 Birth ... Nuchal Translucency at 12 weeks - YouTube
Nuchal Translucency at 12 weeks - YouTube Nuchal translucency scan - 12 week scan, down's syndrome screening.
Nuchal translucency scan - 12 week scan, down's syndrome screening. Nuchal Scan: First Trimester Screening, Results: Normal Range ...
Nuchal Scan: First Trimester Screening, Results: Normal Range ... 12 week NT scan, boy or girl????
12 week NT scan, boy or girl???? Nuchal Translucency Scan | Queensland X-Ray
Nuchal Translucency Scan | Queensland X-Ray 12-week pregnancy dating scan: what will it tell me? - MadeForMums
12-week pregnancy dating scan: what will it tell me? - MadeForMums Nuchal Translucency Ultrasound | Advanced Women's Imaging
Nuchal Translucency Ultrasound | Advanced Women's Imaging Love, Marriage and The Elusive Baby Carriage: NT Scan at 12 Weeks
Love, Marriage and The Elusive Baby Carriage: NT Scan at 12 Weeks NT Scan – 12 weeks 4 days!! | Our Journey through life
NT Scan – 12 weeks 4 days!! | Our Journey through life Can't get an accurate nuchal translucency measurement? Don't let ...
Can't get an accurate nuchal translucency measurement? Don't let ... 12 week NT scan, any gender guesses? - BabyCenter
12 week NT scan, any gender guesses? - BabyCenter 12 week 4 day sono....NT SCAN - YouTube
12 week 4 day sono....NT SCAN - YouTube 12 week NT scan and just found out we are having TWINS! - January ...
12 week NT scan and just found out we are having TWINS! - January ... Normal Values for the Nuchal Translucency and Technique for ...
Normal Values for the Nuchal Translucency and Technique for ... Normal nuchal translucency measurement ( arrows ) at 12 weeks, 5 ...
Normal nuchal translucency measurement ( arrows ) at 12 weeks, 5 ...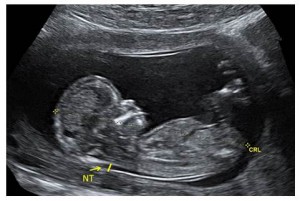 Nuchal Translucency Ultrasound - Prenatal Screening Ontario
Nuchal Translucency Ultrasound - Prenatal Screening Ontario Nuchal Translucency
Nuchal Translucency Do you see the nub? 12 week NT scan. — The Bump
Do you see the nub? 12 week NT scan. — The Bump Nuchal Translucency Measurement 11 weeks - September 2018 Babies ...
Nuchal Translucency Measurement 11 weeks - September 2018 Babies ... NT Scan: What You'll Find Out
NT Scan: What You'll Find Out The 11-14-week scan - Chapter 1
The 11-14-week scan - Chapter 1 13.4 week NT scan – between leg shot – boy?? :)
13.4 week NT scan – between leg shot – boy?? :) Crazy Infertile: 12 Week NT Scan
Crazy Infertile: 12 Week NT Scan The detection of spina bifida at 11–13+6 weeks' gestation - Borg ...
The detection of spina bifida at 11–13+6 weeks' gestation - Borg ... 12 weeks 6 days NT scan Boy or girl?? - August 2017 - BabyCenter ...
12 weeks 6 days NT scan Boy or girl?? - August 2017 - BabyCenter ... 12 Week Scan | SO + GI Scan
12 Week Scan | SO + GI Scan Dating scan accuracy 12 weeks | 12 Week NT scan fetal nuchal ...
Dating scan accuracy 12 weeks | 12 Week NT scan fetal nuchal ... 3d 12 week nt scan…boy or girl? Please guess ;) in Ultrasound ...
3d 12 week nt scan…boy or girl? Please guess ;) in Ultrasound ... Gender Prediction during NT SCAN! - February 2019 Babies | Forums ...
Gender Prediction during NT SCAN! - February 2019 Babies | Forums ... The New Prospective Parenthood: When Does More Info Become Too ...
The New Prospective Parenthood: When Does More Info Become Too ... 12 Week Scan | SO + GI Scan
12 Week Scan | SO + GI Scan Nuchal translucency scan | Pregnancy Birth and Baby
Nuchal translucency scan | Pregnancy Birth and Baby NT Scan and testing for Down Syndrome | Cirque de Baby
NT Scan and testing for Down Syndrome | Cirque de Baby How to perform Nuchal Translucency Scan - YouTube
How to perform Nuchal Translucency Scan - YouTube Bump Watch: The 12 Week Scan | Edspire
Bump Watch: The 12 Week Scan | Edspire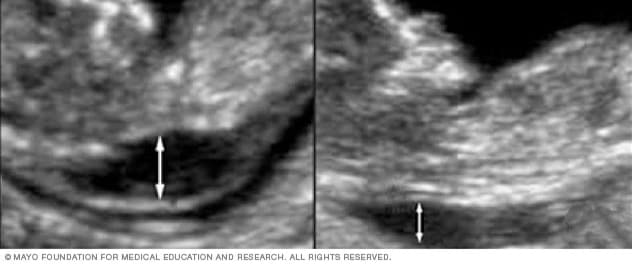 First trimester screening - Mayo Clinic
First trimester screening - Mayo Clinic Nuchal Scan | Paras
Nuchal Scan | Paras Nuchal Translucency Scan – The 411 | Plan B Chronicles
Nuchal Translucency Scan – The 411 | Plan B Chronicles 12 Weeks Pregnant Ultrasound: Process, Abnormalities & Accuracy
12 Weeks Pregnant Ultrasound: Process, Abnormalities & Accuracy Nuchal translucency: an ultrasound marker for fetal chromosomal ...
Nuchal translucency: an ultrasound marker for fetal chromosomal ... The discovery | Ultrasound, 12 week ultrasound, 12 week scan
The discovery | Ultrasound, 12 week ultrasound, 12 week scan 12 Week NT Scan - All is Good!! - tomofam
12 Week NT Scan - All is Good!! - tomofam The 11-14-week scan - Chapter 2
The 11-14-week scan - Chapter 2 Team Sandness: 12 Week Ultrasound Nuchal Translucency (NT) Scan
Team Sandness: 12 Week Ultrasound Nuchal Translucency (NT) Scan
Posting Komentar
Posting Komentar