 Late-onset GBS Disease - Group B Strep International
Late-onset GBS Disease - Group B Strep International© 1996-2018 MedicineNet, Inc. All rights reserved.
MedicineNet does not provide medical advice, diagnosis or treatment. ,
/// / group b strep article
Group B streptococcus (GBS) is a type of bacteria that can exist in the female reproductive tract without causing symptoms. Up to 30% of healthy women carry group B streptococcus can, and usually does not cause problems. However, sometimes it can cause serious infections of the bloodstream, the infection of the placenta, or urinary tract infection. Group B strep can also have serious consequences for the baby, causing potentially life-threatening infections in newborns, including meningitis, pneumonia, and sepsis. This test is usually performed between 35 and 37 weeks of pregnancy and should be done in a subsequent pregnancy even if you test negative on your first pregnancy.
Group B (GBS) is a type of gram-positive streptococcus bacteria, also known as Streptococcus agalactiae. This type of bacteria (not to be confused with, the cause) is commonly found in (this is called colonization), and usually do not cause any symptoms. However, in certain cases, can be the cause of dangerous infections that can affect nonpregnant adults, pregnant women, and their newborn baby. In the United States, approximately 30,800 cases of invasive GBS disease occur each year in all age groups. Group B disease is the most common cause of neonatal sepsis and in the United States.
Group B streptococcal infection can also override nonpregnant adults with chronic medical conditions, such as ,,, and. The incidence of group B streptococcal disease in adults increases with age, with the highest rates in adults aged 65 years and older (25 cases per 100,000). Although the incidence of neonatal group B infections have declined, the incidence of GBS infections in nonpregnant adults has increased.
Group B strep bacteria can usually be found in approximately 25% -30% of all pregnant women healthy. Group B strep is commonly found in the intestines, vagina and anal area. Most women who are carriers of the bacteria (colonized) will not have any symptoms; However, in certain circumstances, perinatal group B strep infection of the mother and / or newborn may develop. In newborns, if the developing GBS infection in the first week of life, it is called early-onset disease. If GBS infection developing from 1 week to 3 months of age, it is referred to as late onset disease. On average, about 1,000 babies in the United States develop early onset disease each year, with the same rate for late onset diseases. According to the Centers for Disease Control and Prevention (CDC), early onset infection rate decreased from 1.7 per 1,000 live births in 1993 to 0.22 cases per 1,000 births in 2016.
in newborns, group B Streptococcus infection acquired through direct contact with the bacteria while in the womb or during birth; thus, pregnancy bacterial infection transmitted from mother to her newborn colonized. Approximately 50% of colonized mothers will pass the bacteria to their babies during and vaginal birth. However, not all infants are affected by bacteria, and statistics show that about one out of every 200 babies born to a mother GBS-colonized really will continue to develop GBS infection.
Group B strep infections are more common in African Americans than in whites. There is also the risk factors mother increases the likelihood of transmission of group B Streptococcus for newborn infants that leads to the disease early onset:
End infection GBS onset occurs more often in babies who were born prematurely (<37 weeks) and in infants whose mothers tested positive for GBS during pregnancy.
Group B strep infection is not ().
in newborns with early-onset GBS infection, signs and symptoms usually develop within the first 24 hours after birth. Infants who experience late onset GBS infection is often healthy and growing, with signs and symptoms of disease develops after the first week of life. Signs and symptoms that can be observed with infection GBS in infants include
For adults who have infections GBS invasive develop
Sources right of group B streptococcal disease in nonpregnant adults often do not determined.
Group B strep infections can be diagnosed and treated by different specialists, depending on the age of the patient and potential complications faced by patients. In pregnant women, GBS infections can be diagnosed and treated during the patient's obstetrician / gynecologist or family physician if they deliver the baby. Infants who develop GBS infection will be treated by a pediatrician or neonatologist, and sometimes infectious disease specialists may be involved. nonpregnant adults who develop GBS infection will often treated by their family doctor, internist, or an infectious disease specialist, and rarely by a general surgeon or orthopedic if skin or bone infections that require surgery are present.
in newborns and adults, GBS bacterial isolation needed for definitive diagnosis. Laboratory studies that isolate the organism from certain body fluids, such as blood, cerebrospinal fluid (CSF), and urine, help establish the diagnosis. For the screening of pregnant women, a health care professional will obtain a swab area of the vagina and rectum to screen women for GBS infection at 35-37 weeks of pregnancy. The test results may take several days. A () may be necessary when meningitis is suspected. A health care professional such order in May imaging to evaluate whether the present.
By clicking "Submit," and I agree with MedicineNet. I also agree to receive emails from MedicineNet and I understand that I can get out of MedicineNet subscription at any time.
For women who test positive for GBS during pregnancy and to those who have certain risk factors for developing or transmitting infection of GBS during pregnancy, intravenous antibiotics are recommended at the time of delivery. Giving antibiotics to women before childbirth is known colonized with GBS is not effective in preventing early onset disease, as it has been discovered that the GBS bacteria can grow back quickly. Pregnant women with GBS isolated from the urine at any time during pregnancy and women who have had a previous infant with invasive GBS infection should receive antibiotics during labor, and thus does not require routine GBS screening at 35-37 weeks of pregnancy. Pregnant women who are unaware of group B strep their status should be given antibiotics during labor if they develop preterm birth (less than 37 weeks gestation), if they have a membrane rupture for 18 hours or more, or if they have a fever during labor. or is the recommended antibiotic, penicillin while individuals can be given either cefazolin, or. Administration of antibiotics has been found to significantly reduce infection early onset GBS in newborns; However, it did not prevent late onset GBS infection. If a pregnant carrier GBS receive intravenous antibiotics during labor, the baby has a one in 4,000 possibility of developing GBS infection. Without antibiotics, the baby has a one in 200 chance of developing GBS infection.
In neonates and nonpregnant adults who develop invasive group B streptococcal disease, intravenous antibiotics are also the mainstay of treatment. There are certain conditions associated with invasive GBS infections that may require surgical intervention, eg, debridement in certain patients with soft tissue / skin / bone infection.
invasive GBS infections in infants can lead to sepsis, pneumonia, meningitis, or sometimes death. In some babies who survive, long-term sequelae of this disease include deafness, or a developmental disability.
In pregnant women, GBS infections can cause infection of the uterus and placenta, as well as premature birth, fetal death, or.
In nonpregnant adults with chronic medical conditions who develop invasive GBS infection, complications may include pneumonia, urinary tract infections, sepsis, skin and soft tissue infections, bone and joint infections, and rarely meningitis.
GBS infection prognosis varies depending on various factors, including the patient's age and the presence of underlying medical conditions. In the United States, the death rate (mortality) for infants with GBS infection is approximately 5%. Pregnant women who are experiencing symptoms of GBS infection also has a low mortality rate, because they tend to be healthy. nonpregnant adults who develop invasive GBS infectsions tend to have higher mortality rates, ranging from 5% -47% depending on the study, as these patients tend to be older and they often have a serious underlying medical condition.
at this point in time, the best measure to prevent GBS infection is through routine checks during pregnancy. This test has served to reduce the overall number of early onset GBS infection in newborns about 80% since an aggressive preventive measures were instituted in the 1990s. In pregnant women, routine screening for GBS colonization with highly recommended. This screening test is done between 35-37 weeks of pregnancy. This test involves using a sterile swab to collect a sample of the vagina and rectum, with results usually available within 24-72 hours.
administration of antibiotics during labor to pregnant women colonized with GBS and for those with risk factors outlined above can help to reduce transmission of infection GBS, and thus decrease the incidence of GBS disease early onset in the newborn.
Although there are currently no licensed available for prevention of GBS infection, there is research under way to try to develop one to use in the future. Further information about the GBS can be found at the Center for Disease Control and Prevention website (https://www.cdc.gov/groupbstrep/index.html).
Congestive heart failure (CHF) refers to a condition in which heart loses its ability to function properly. heart disease, high blood pressure, diabetes, myocarditis and cardiomyopathy only a few potential causes congestive heart failure.
The signs and symptoms of congestive heart failure may include fatigue, shortness of breath, palpitations, angina, and edema. physical examination, patient history, blood tests, and imaging tests are used to diagnose congestive heart failure.
Treatment of heart failure consists of a modification of lifestyle and taking medication to reduce fluid in the body and reduce the strain on the heart. The prognosis of patients with congestive heart failure depends on the stage of heart failure and the overall condition of the individual.
© 1996-2020 MedicineNet, Inc. All rights reserved.
MedicineNet does not provide medical advice, diagnosis or treatment. ,
 Group B Strep (GBS) During Pregnancy: Risks to the Baby
Group B Strep (GBS) During Pregnancy: Risks to the Baby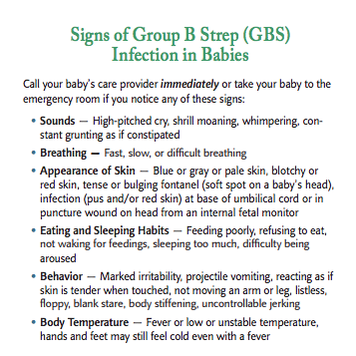 Sebastian's Story - Group B Strep International
Sebastian's Story - Group B Strep International Know the symptoms of group B Strep... - Group B Strep Support ...
Know the symptoms of group B Strep... - Group B Strep Support ... Poster - Symptoms of group B Strep infection in babies
Poster - Symptoms of group B Strep infection in babies Symptoms of group B Strep infection in babies poster by Group B ...
Symptoms of group B Strep infection in babies poster by Group B ... Group B strep
Group B strep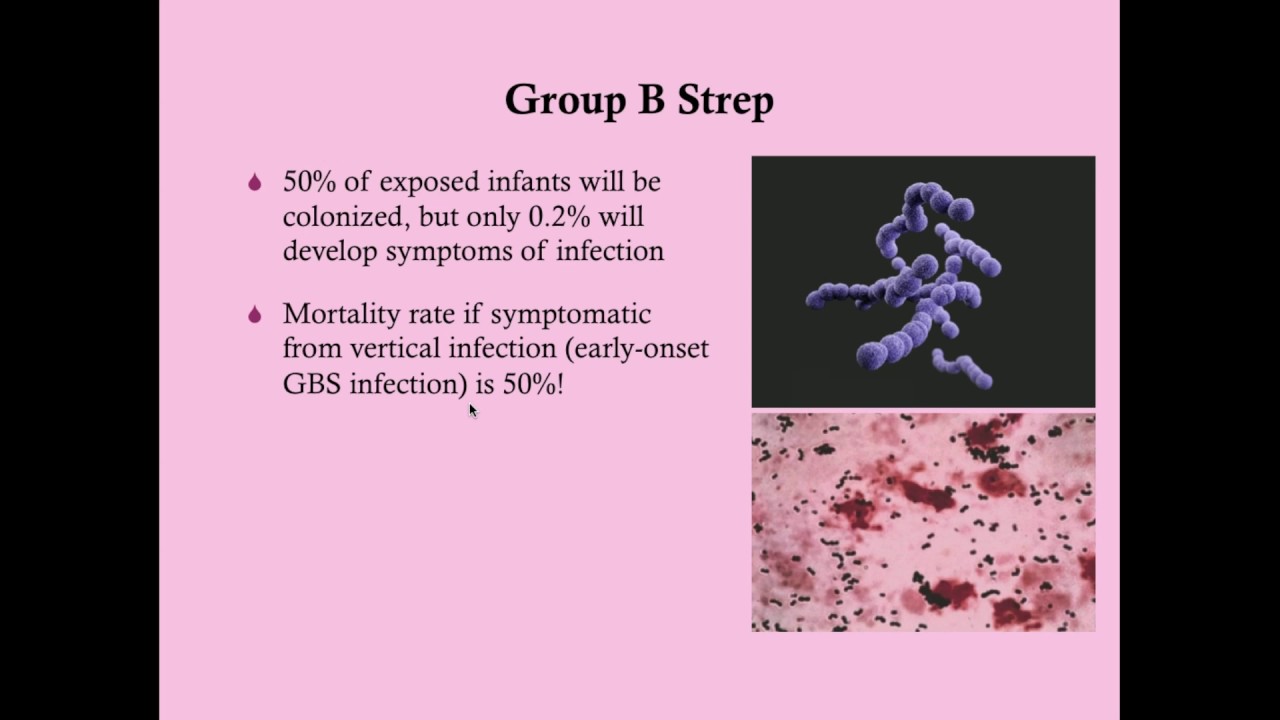 Group B Strep in Pregnancy - CRASH! Medical Review Series - YouTube
Group B Strep in Pregnancy - CRASH! Medical Review Series - YouTube Group b strep yeast infection treatment symptoms - onvv.hmgroup.pro
Group b strep yeast infection treatment symptoms - onvv.hmgroup.pro Prevention of Perinatal Group B Streptococcal Disease: Updated CDC ...
Prevention of Perinatal Group B Streptococcal Disease: Updated CDC ...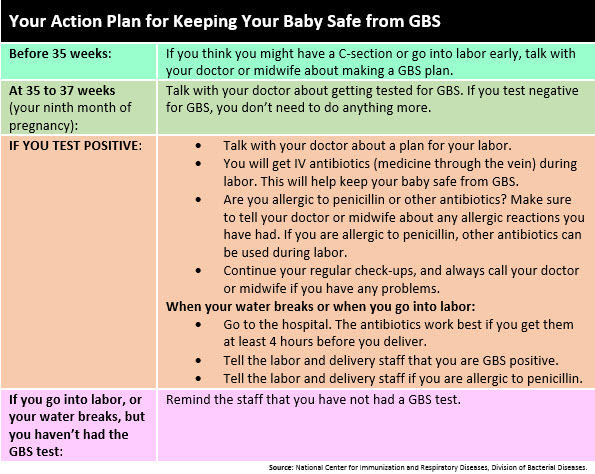 Goldsboro Pediatrics - Tip of the Week
Goldsboro Pediatrics - Tip of the Week Group B strep
Group B strep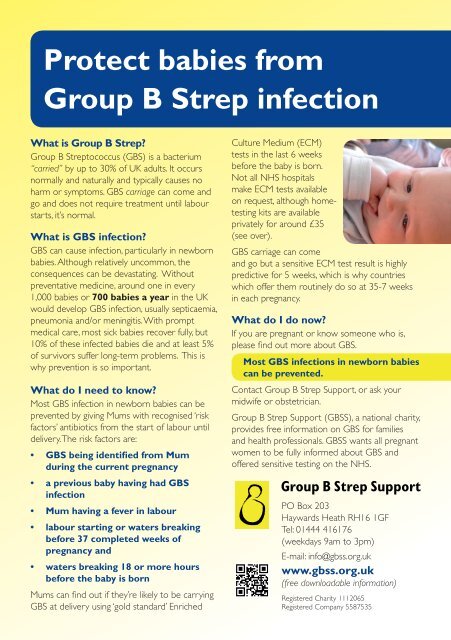 Protect babies from Group B Strep infection - Group B Strep Support
Protect babies from Group B Strep infection - Group B Strep Support Treating GBS During First Trimester? - BabyCenter
Treating GBS During First Trimester? - BabyCenter July is International Group B Strep Awareness Month - Group B ...
July is International Group B Strep Awareness Month - Group B ... Poster Pregnant - are you group B Strep aware?
Poster Pregnant - are you group B Strep aware?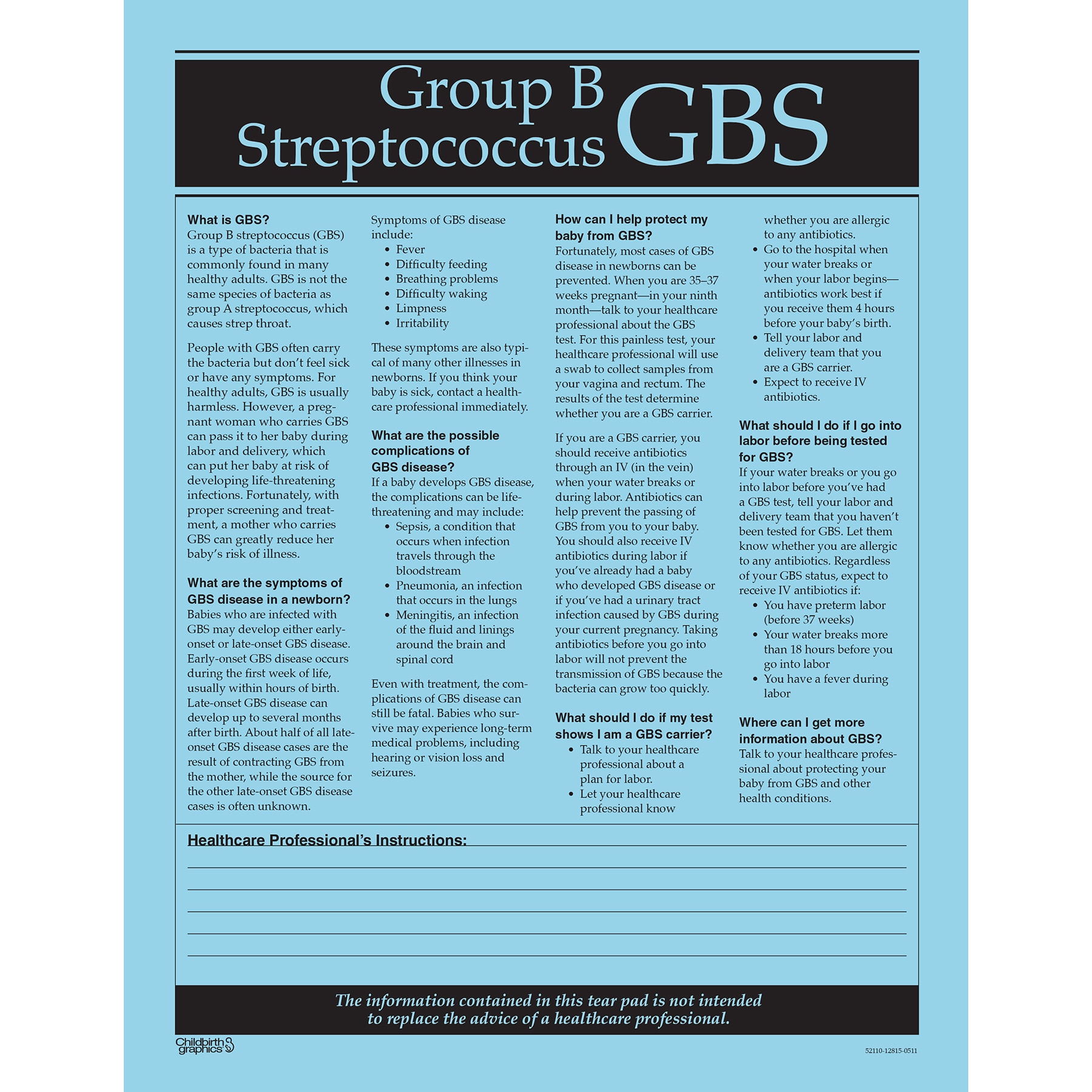 Group B Streptococcus (GBS) Tear Pad | Childbirth Graphics
Group B Streptococcus (GBS) Tear Pad | Childbirth Graphics Protect babies from group b strep infection leaflet by Group B ...
Protect babies from group b strep infection leaflet by Group B ... Group B streptococcal infection - Wikipedia
Group B streptococcal infection - Wikipedia Streptococcus Group B - Infectious Disease and Antimicrobial Agents
Streptococcus Group B - Infectious Disease and Antimicrobial Agents Group b strep - February 2019 Babies | Forums | What to Expect
Group b strep - February 2019 Babies | Forums | What to Expect I Tested GBS Positive, Now What? - B I R T H F I T
I Tested GBS Positive, Now What? - B I R T H F I T Group B Streptococcal Infections | American Academy of Pediatrics
Group B Streptococcal Infections | American Academy of Pediatrics Streptococcus agalactiae (group B strep)- causes, symptoms ...
Streptococcus agalactiae (group B strep)- causes, symptoms ... Prevention of Perinatal Group B Streptococcal Disease
Prevention of Perinatal Group B Streptococcal Disease Streptococcus Group B - Infectious Disease and Antimicrobial Agents
Streptococcus Group B - Infectious Disease and Antimicrobial Agents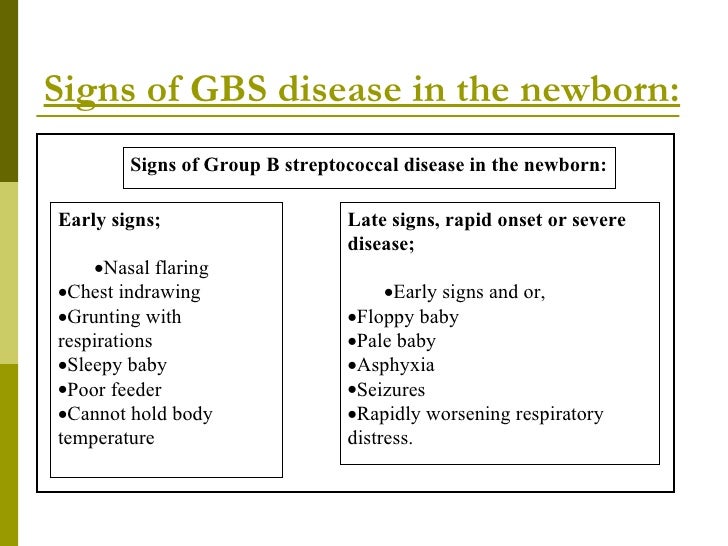 Gbs
Gbs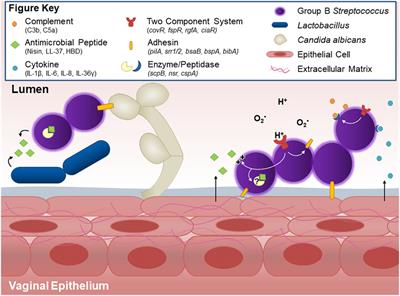 Frontiers | Group B Streptococcal Maternal Colonization and ...
Frontiers | Group B Streptococcal Maternal Colonization and ... GBS | Prevention in Newborns | Group B Strep | CDC
GBS | Prevention in Newborns | Group B Strep | CDC Group B strep: What to know in adults and babies
Group B strep: What to know in adults and babies CDC Updates Guidelines for the Prevention of Perinatal GBS Disease ...
CDC Updates Guidelines for the Prevention of Perinatal GBS Disease ... Group B Strep in numbers infographic by Group B Strep Support - issuu
Group B Strep in numbers infographic by Group B Strep Support - issuu Image result for rectal strep | Rectal, Sexually transmitted ...
Image result for rectal strep | Rectal, Sexually transmitted ... Group B Strep meningitis | Meningitis Now
Group B Strep meningitis | Meningitis Now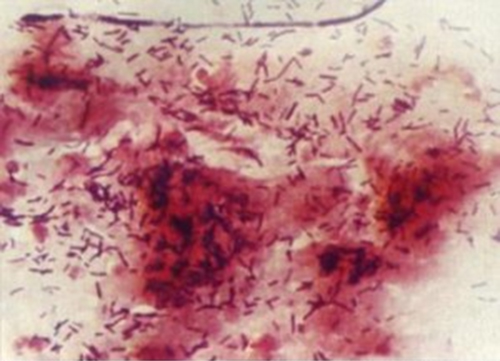 Group B Streptococcus | Health, Seniors and Active Living ...
Group B Streptococcus | Health, Seniors and Active Living ... Specific Bacterial Infections: Group B Streptococcus | GLOWM
Specific Bacterial Infections: Group B Streptococcus | GLOWM Group B Streptococcal Infections | American Academy of Pediatrics
Group B Streptococcal Infections | American Academy of Pediatrics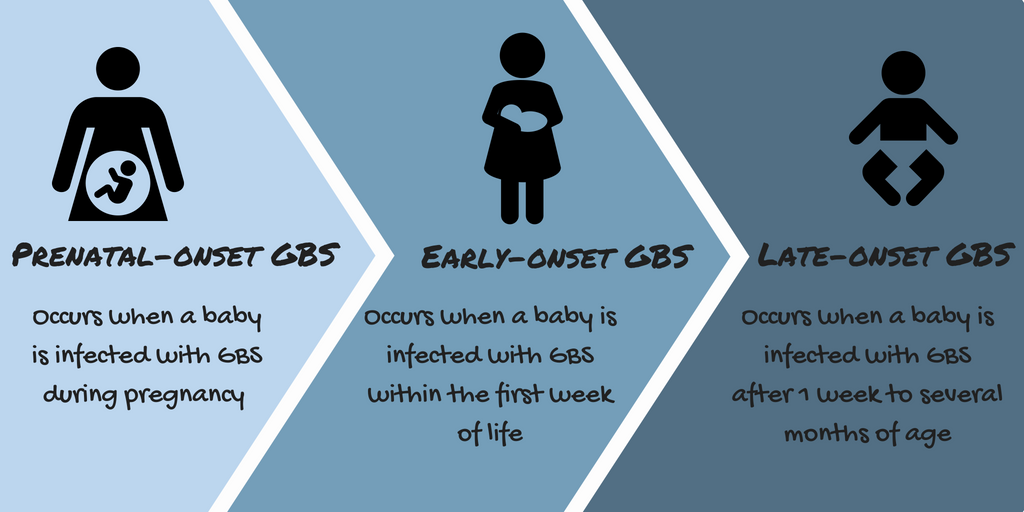 Awareness as the first step to prevention: prenatal infection and ...
Awareness as the first step to prevention: prenatal infection and ... Info Sheet: Group B Strep Test
Info Sheet: Group B Strep Test Streptococcus agalactiae (Group B Strep; GBS; Sample Page ...
Streptococcus agalactiae (Group B Strep; GBS; Sample Page ... What Is Group B Strep? - Group B Strep International
What Is Group B Strep? - Group B Strep International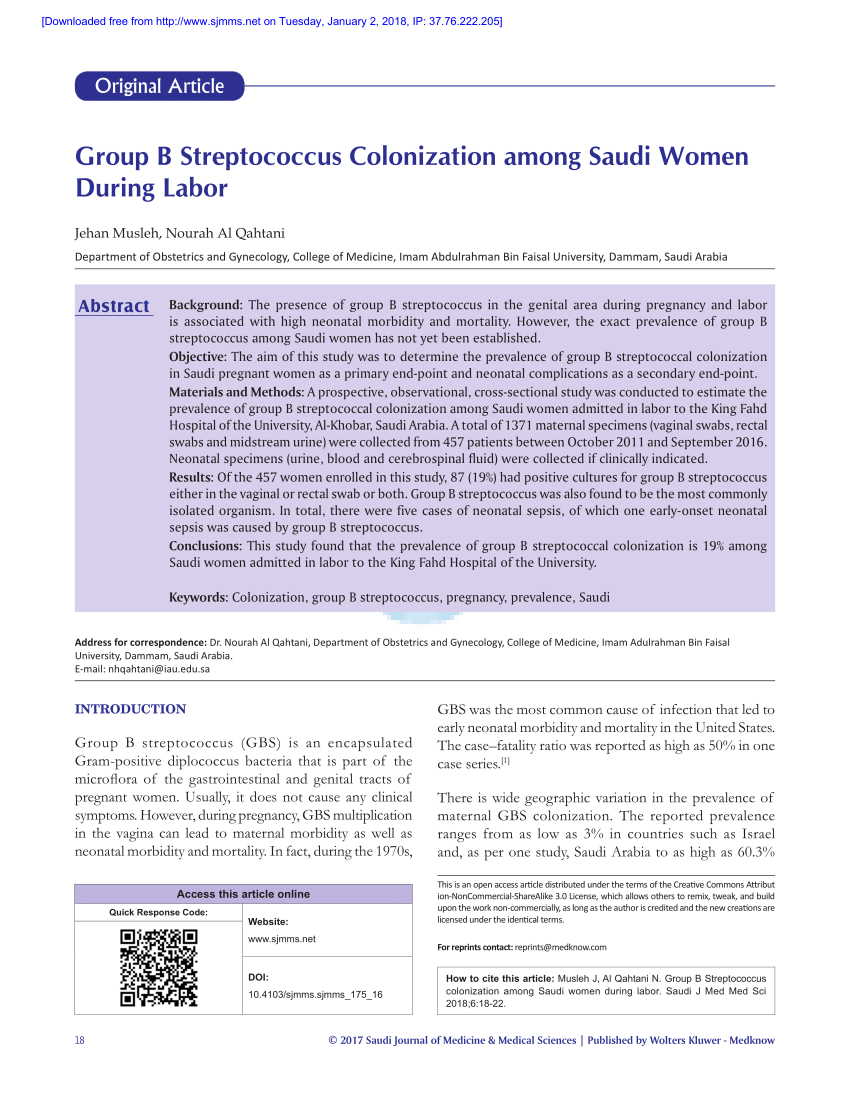 PDF) Group B Streptococcus Colonization among Saudi Women During Labor
PDF) Group B Streptococcus Colonization among Saudi Women During Labor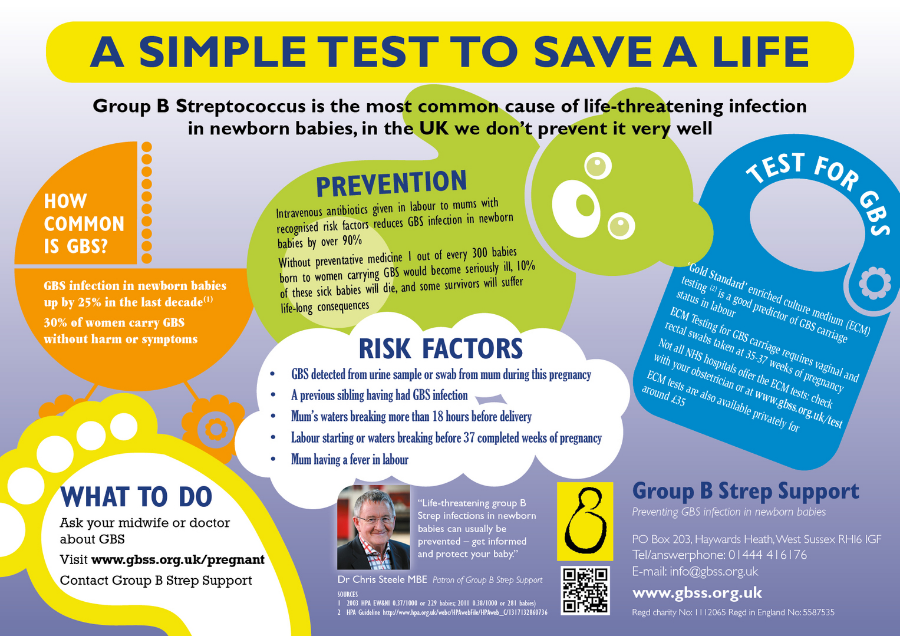 The Faith Cause: Increasing Group B Strep Awareness - Are you ...
The Faith Cause: Increasing Group B Strep Awareness - Are you ...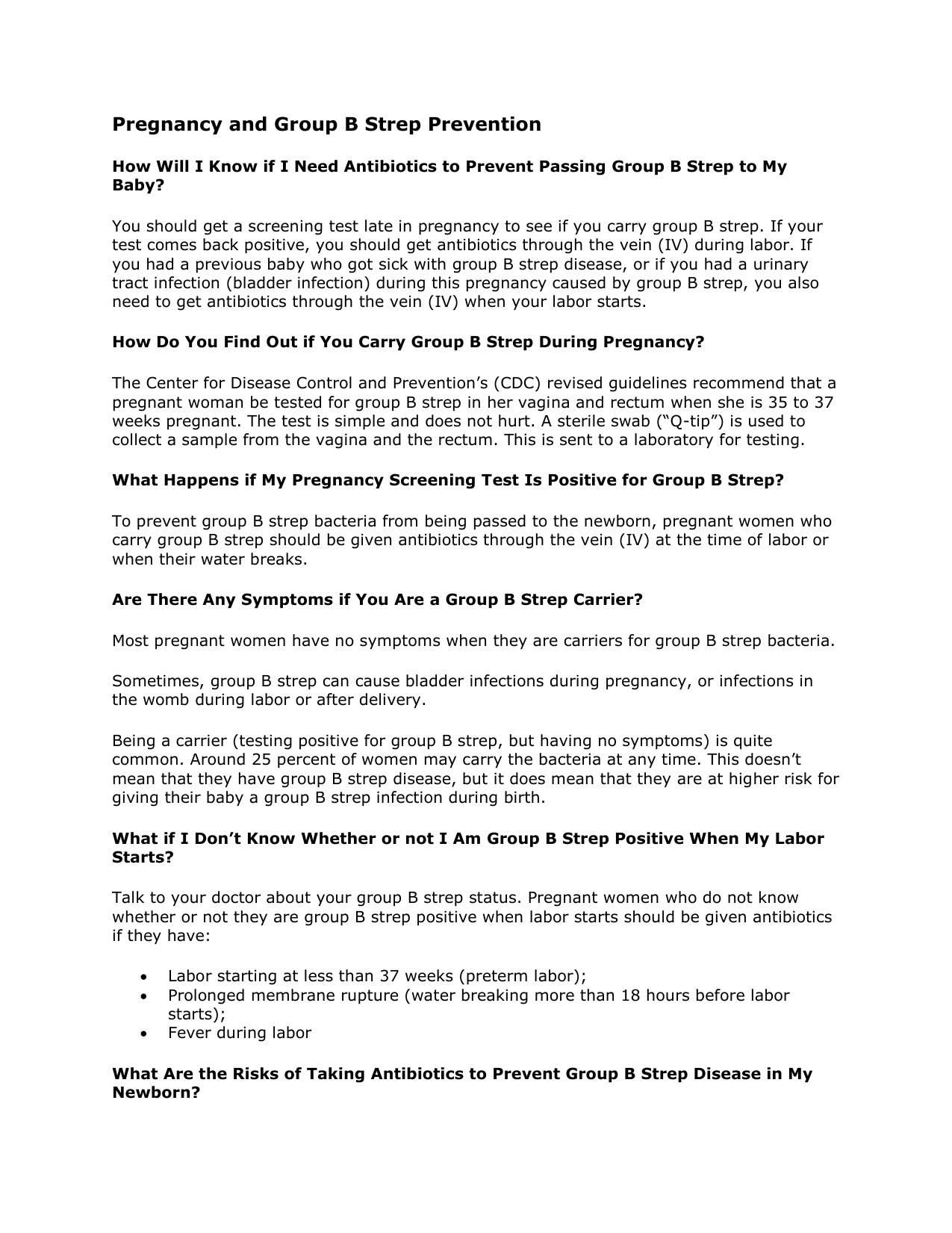 Pregnancy and Group B Strep Prevention
Pregnancy and Group B Strep Prevention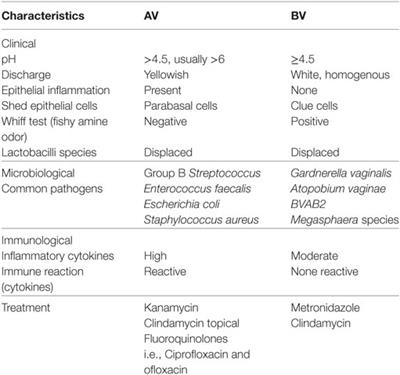 Frontiers | Vaginal Microbiomes Associated With Aerobic Vaginitis ...
Frontiers | Vaginal Microbiomes Associated With Aerobic Vaginitis ...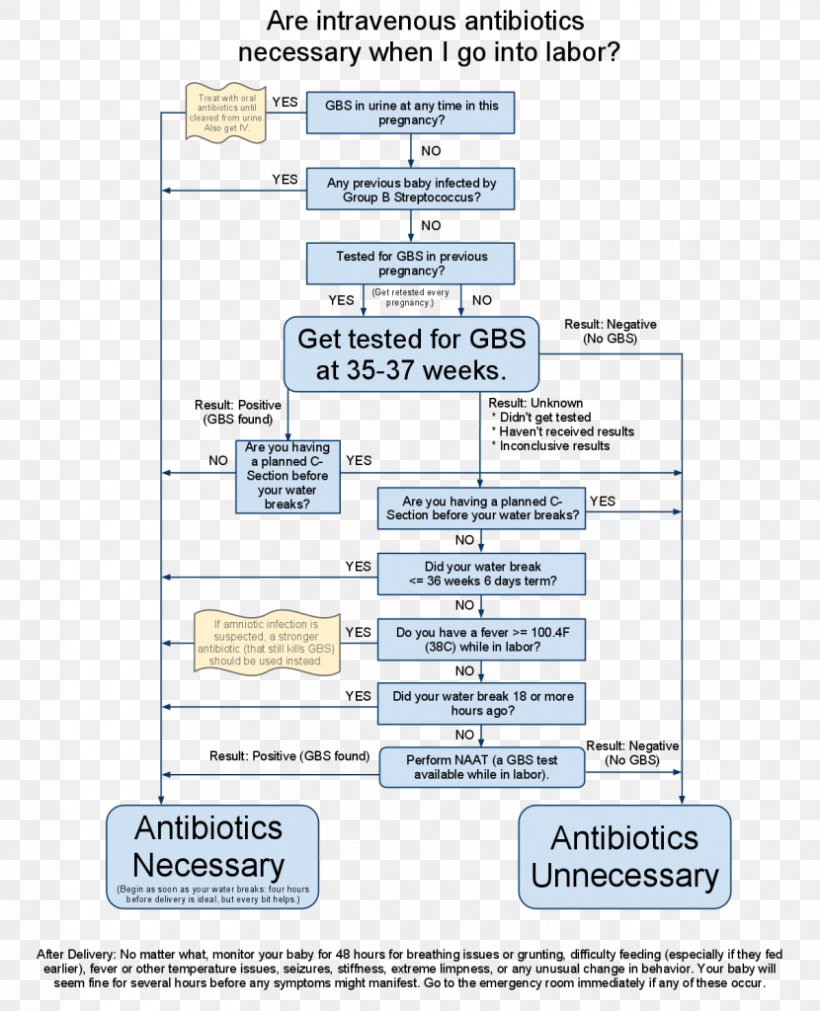 Group B Streptococcal Infection Streptococcus Antibiotics ...
Group B Streptococcal Infection Streptococcus Antibiotics ... Streptococcus Group B - Infectious Disease and Antimicrobial Agents
Streptococcus Group B - Infectious Disease and Antimicrobial Agents Prevention of Perinatal Group B Streptococcal Disease
Prevention of Perinatal Group B Streptococcal Disease Group B streptococcal infection - Wikipedia
Group B streptococcal infection - Wikipedia Prevention of Neonatal Group B Streptococcal Infection - American ...
Prevention of Neonatal Group B Streptococcal Infection - American ... How to beat group b strep for good
How to beat group b strep for good Epidemiology of Group B Streptococcal Disease in the United States ...
Epidemiology of Group B Streptococcal Disease in the United States ... Group B Strep In Pregnancy - 2015 - Journal of Midwifery & ...
Group B Strep In Pregnancy - 2015 - Journal of Midwifery & ...
Posting Komentar
Posting Komentar