 Breech pregnancy | Pregnancy Birth and Baby
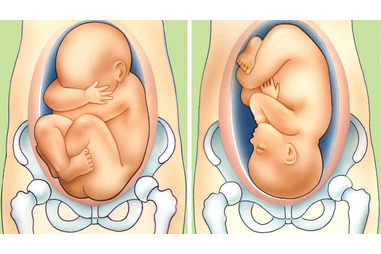
Breech pregnancy | Pregnancy Birth and BabyWith about 8 months, there is not much space in the uterus. Most babies maximize their cramped quarters with settling in a head-down, in what is known as cephalic presentation. But if your baby is breech, it means he is ready to come out buttocks or feet first.
When labor begins at term (37 weeks or more), almost 97 percent of infants are set to come out head first. Most of the rest was breech. (In rare cases, the baby will be sideways in the womb with his shoulder, back, or arms present a first -. This is called a lie crosswise)
There are several types of breech presentation, including breech frank (bottom first with feet near the head), complete breech (bottom first with legs crossed Indian style), or stupid breech (one or both legs are ready to come out first). See.
At the beginning of the third trimester, your doctor may be able to tell what position your baby in your belly to feel and find the baby's head, back, and bottom. About a quarter of babies are breech at the moment, but most will turn on their own over the next two months.
If you do not clear the baby's position during abdominal examination at 36 weeks, your caregiver may do an internal examination to try to feel what part of the baby in your pelvis. In some cases, he may use ultrasound to confirm the position of the baby.
Babies who are breech near future is unlikely to turn on their own. So, if your baby is still down below at 37 weeks, your caregiver should offer to try to change your baby with the head down position which is more favorable, assuming you are a proper candidate.
This procedure is known as external cephalic version (ECV). This is done by applying pressure to your stomach and manually manipulate the baby to the head-down position. (If the caregiver you are not experienced in this procedure, he may refer you to someone who is.)
ECV has about a success rate of 58 percent in turning breech babies (and a success rate of 90 percent if the baby is a lie athwart .) But sometimes the baby refused to relent or turn back to the breech position after a successful version. ECV is more likely to work if this is not your first baby.
Not all women can have ECV. If you are carrying twins or your pregnancy complicated by bleeding or you will not be able to have the procedure. And, of course, you will not have a version if you will deliver by caesarean anyway - for example, if you have, triplets, or more than one prior c-section
severe complications, while relatively rare, can occur. For example, an ECV can cause the placenta to separate from the uterine wall so that your baby has to be delivered directly by c-section. The procedure also causes a decrease in your baby's heart rate, which, if not quickly resolve themselves, would require immediate delivery.
For this reason, doctors must perform the procedure in the hospital with the facilities and staff available for an emergency c-section in case any complications arise. You will be told not to eat or drink anything after midnight the night before the procedure, in case you end up needing surgery.
When you go, you will have blood drawn and IV may begin. Rh-negative women who have to get an injection of Rh immune globulin to the procedure unless the baby's father is Rh-negative. Your baby's heartbeat will be monitored for the time before and after the procedure.
You will have an ultrasound beforehand to check your baby's position, placental location, and the amount of amniotic fluid. Ultrasound will be repeated after the maneuver is done. (Some doctors also use ultrasound during the procedure.)
Several studies show a higher success rate for ECV when uterine-relaxing drug use.
It depends. You may have a vaginal breech delivery if you have a twin pregnancy in which the first baby is in a first position and a second baby's head is not, or if your work force so rapidly that you arrived at the hospital just about to deliver.
However, most babies are breech stay comes with a c-section. A large international study published in 2000 showed that a planned c-section results in the safest results for a single baby is breech. The following year the American College of Obstetricians and Gynecologists (ACOG) issued Opinion Committee advises against a planned vaginal delivery of the baby.
Longer-term follow-up of infants in this study led the researchers to question this conclusion. And other recent reports indicate that certain patients may have a safe vaginal delivery. This includes women whose pelvic seemed quite large, the labor started and develop properly its own, and whose babies were honest-term or full pants and seemingly average weight with no abnormalities shown by ultrasound.
In recognition of these studies, ACOG issued a new Opinion Committee in July 2006. This time the organization noted that it may be appropriate for some women to plan for a normal delivery. ACOG warns that caregivers need to be experienced in performing vaginal breech delivery (fewer and fewer of them) and women should be made aware that the risk to the baby may be higher than with a planned cesarean.
If a planned c-section, which is likely for most women, usually will be scheduled for no earlier than 39 weeks. To make sure your baby's position has not changed in the meantime, you will have an ultrasound at the hospital to confirm his position before the operation.
There is also the possibility that you will go into labor or your water will break before a planned c-section. If that happens, be sure to contact your provider immediately and head for the hospital.
Here are some alternative methods you may hear about. There is no evidence that any of them work or even safe. Consult a doctor before trying them.
 Breech birth | BabyCenter
Breech birth | BabyCenter What is the breech position, what happens when a baby is breech ...
What is the breech position, what happens when a baby is breech ... Breech Presentation - Breech Births
Breech Presentation - Breech Births What does 'breech baby' mean, and will a breech baby turn? – My ...
What does 'breech baby' mean, and will a breech baby turn? – My ... Is Baby in a Breech Position? How to Tell & What to Do | Breech ...
Is Baby in a Breech Position? How to Tell & What to Do | Breech ... Breech Baby |Reasons for Breech Baby position|Delivery of Breech Baby
Breech Baby |Reasons for Breech Baby position|Delivery of Breech Baby Cerebral Palsy Caused by Breech Presentation | Legal Help
Cerebral Palsy Caused by Breech Presentation | Legal Help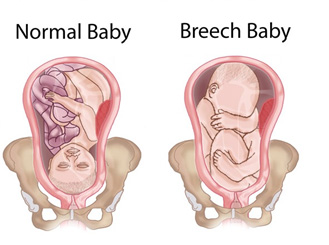 Breech breast milk vomiting acupuncture treatment Nashik
Breech breast milk vomiting acupuncture treatment Nashik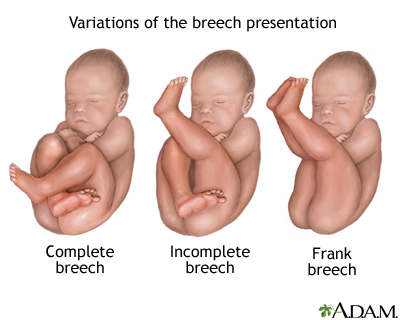 Breech - series—Types of breech presentation: MedlinePlus Medical ...
Breech - series—Types of breech presentation: MedlinePlus Medical ... 7 ways to turn a breech baby
7 ways to turn a breech baby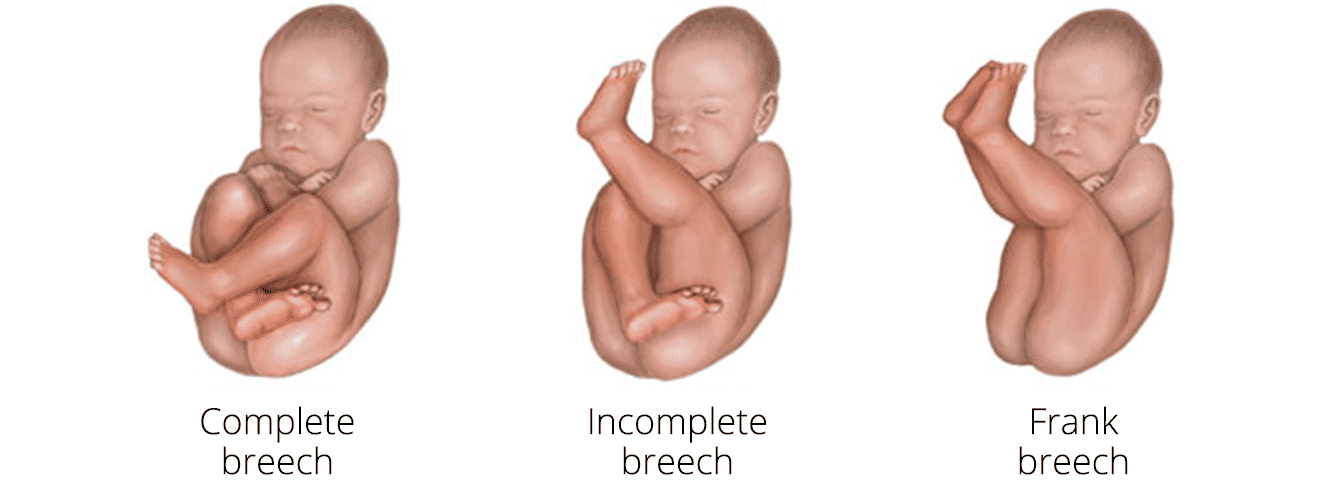 Breech baby — Chelsea and Westminster Hospital NHS Foundation Trust
Breech baby — Chelsea and Westminster Hospital NHS Foundation Trust How To Turn A Breech Baby | Vicki Hobbs
How To Turn A Breech Baby | Vicki Hobbs If Your Baby is Breech | Birth International
If Your Baby is Breech | Birth International.jpg) RANZCOG - Breech Presentation at the End of your Pregnancy
RANZCOG - Breech Presentation at the End of your Pregnancy Turning a Breech Baby: Care Instructions
Turning a Breech Baby: Care Instructions Summit Medical Group
Summit Medical Group Is a breech delivery at term (37+ weeks) dangerous for me or the baby?
Is a breech delivery at term (37+ weeks) dangerous for me or the baby? What is the breech position, what happens when a baby is breech ...
What is the breech position, what happens when a baby is breech ... How To Deliver a Baby In Breech Position | Delivering a baby, Baby ...
How To Deliver a Baby In Breech Position | Delivering a baby, Baby ... What does 'breech baby' mean, and will a breech baby turn? – My ...
What does 'breech baby' mean, and will a breech baby turn? – My ... Breech Baby: Causes, Complications, and Turning
Breech Baby: Causes, Complications, and Turning Breech birth - Wikipedia
Breech birth - Wikipedia Breech Baby - Breech Birth - Position of Baby
Breech Baby - Breech Birth - Position of Baby Is Baby in a Breech Position? How to Tell & What to Do
Is Baby in a Breech Position? How to Tell & What to Do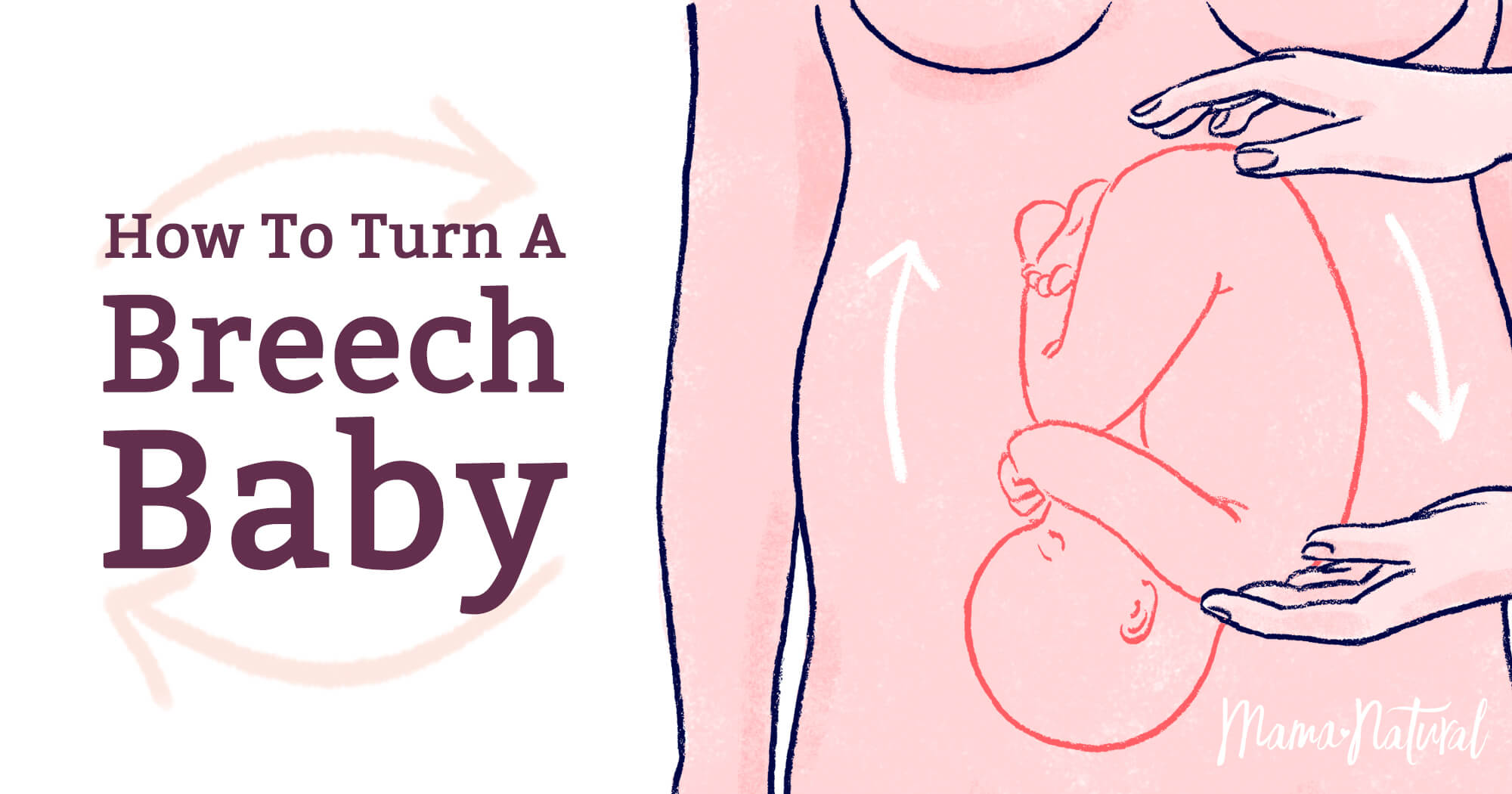 Breech Baby: Techniques for Turning a Breech Baby Naturally
Breech Baby: Techniques for Turning a Breech Baby Naturally Positions, please: how babies' worlds turn
Positions, please: how babies' worlds turn What to Do for a Baby in Breech Position | Parents
What to Do for a Baby in Breech Position | Parents Breech Birth
Breech Birth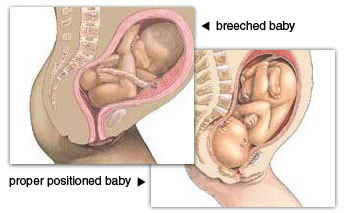 breech | Tumblr
breech | Tumblr What to expect if your baby is in the breech position
What to expect if your baby is in the breech position Breech Baby: Techniques for Turning a Breech Baby Naturally
Breech Baby: Techniques for Turning a Breech Baby Naturally strange question about breech babies - BabyCenter
strange question about breech babies - BabyCenter Breech Baby - A Guide to Breech Presentation - Spinning Babies
Breech Baby - A Guide to Breech Presentation - Spinning Babies Everything you wanted to know about breech birth, but were afraid ...
Everything you wanted to know about breech birth, but were afraid ... Breech Birth - Pregnancy Problems (Pregnancy Health Guru) - YouTube
Breech Birth - Pregnancy Problems (Pregnancy Health Guru) - YouTube How to Turn a Breech Baby at 37 Weeks? Different Breech Positions ...
How to Turn a Breech Baby at 37 Weeks? Different Breech Positions ... How to turn a breech baby - MadeForMums
How to turn a breech baby - MadeForMums Doctor Turns Breech Baby Still in Mother's Belly - YouTube
Doctor Turns Breech Baby Still in Mother's Belly - YouTube What to Do When Your Baby is Breech: Your Breech Pregnancy Guide
What to Do When Your Baby is Breech: Your Breech Pregnancy Guide/98359376-56a770f13df78cf77295f9c5.jpg) Transverse Lie Position in Pregnancy
Transverse Lie Position in Pregnancy How to Help Turn A Breech Baby Naturally | Northeastern Chiropractic
How to Help Turn A Breech Baby Naturally | Northeastern Chiropractic Breech Birth: What Are Your Options for Delivery?
Breech Birth: What Are Your Options for Delivery? 5 Signs Your Baby Is Breech, According To Experts
5 Signs Your Baby Is Breech, According To Experts What is the breech position, what happens when a baby is breech ...
What is the breech position, what happens when a baby is breech ... How to Turn a Breech Baby: 13 Steps (with Pictures) - wikiHow
How to Turn a Breech Baby: 13 Steps (with Pictures) - wikiHow External Cephalic Version (ECV) for breech position at Catharina ...
External Cephalic Version (ECV) for breech position at Catharina ... Breech Baby: Techniques for Turning a Breech Baby Naturally
Breech Baby: Techniques for Turning a Breech Baby Naturally Pin on Family Life
Pin on Family Life Breech babies: what you need to know | NCT
Breech babies: what you need to know | NCT Video: Externally turning a breech baby looks painful...and ...
Video: Externally turning a breech baby looks painful...and ... Complete Guide for Breech Babies - KG Hypnobirthing
Complete Guide for Breech Babies - KG Hypnobirthing Breech Babies: What Can I Do if My Baby is Breech?
Breech Babies: What Can I Do if My Baby is Breech?
Posting Komentar
Posting Komentar