 What to Expect With a Baby Born at 24 Weeks | LoveToKnow
What to Expect With a Baby Born at 24 Weeks | LoveToKnowfetal survival or fetal viability is the ability to survive outside.
Viability, as the word has been used in the United States since the constitutional law, is a potential fetus to survive outside the uterus after childbirth, natural or induced, when supported by the drug up-to-date. viability of the fetus depends on the maturity of fetal organs, and environmental conditions. According to Webster's Encyclopedic Unabridged Dictionary of English, survival means the fetus has reached the stage of development as to be able to live, under normal conditions, outside the womb. Viability exists as a function of biomedical and technological capacity, which is different in different parts of the world. As a result, there is, at present, there is no worldwide, uniform gestational age that defines viability.
According to McGraw-Hill Medical Dictionary nonviable fetus is "expelled or delivered fetus, although live, may not survive to the point of maintaining an independent life, even with the best support available medical therapy." A state law definition :. "Then nonviable not afford to live, grow, or develop and function successfully This is the opposite of decent, defined as has attained the form and become normal organ development as capable of living outside the womb." [Wolfe v. Isbell, 291 Ala. 327, 329 (Ala. 1973)]
Various jurisdictions have different legal definitions of survival. In, under, viability of the fetus is defined as "a point in the pregnancy in which, in the reasonable opinion of a medical practitioner, the fetus is able to survive outside the womb without life-sustaining treatment that is remarkable." [Definitions (Part 2) (8)]
There are no sharp boundaries of development, or the weight in which the human fetus automatically becomes feasible. While there is no limit sharply the development, pregnancy, or weight where the human fetus automatically becomes feasible, a study in 2013 found that "While only a small percentage of births occur before 24 weeks of full (approximately 1 per 1000), survival is rare and most of them are one or a live birth is followed by neonatal mortality. " According to the study between 2003 and 2005, 20 to 35 percent of babies born at 24 survived, while 50 to 70 percent of babies born at 25 weeks, and more than 90 percent are born at 26 to 27 weeks, congratulations.
This belief in the viability of different in each country. medical decisions regarding resuscitation of extremely premature infants (EPI) is considered in the "gray zone" typically take into account body weight and gestational age, as well as the views of parents. One 2018 study showed that there were significant differences between countries in what is considered a "gray zone", "gray zone" is considered 22.0 to 22.6 / 23 weeks in Sweden, 23.0 to 23 , 6/24 weeks in the UK, and 24.0 to 25.6 / 26 weeks in the Netherlands. Is the viability of the fetus in the period may have legal consequences as far as the protection of the rights of the fetus is concerned. Traditionally, the period of viability referred to the period after the twenty-eighth week,
expressed in (1973) viability (ie, "interim point in which the fetus becomes ... potentially able to live outside the mother's womb, albeit with artificial aid") "is usually placed at about seven months (28 weeks) but may occur earlier, even at 24 weeks. " Definition of 28-weeks of being part of a "framework trimester" marks the point where the "interests of the state" (under the doctrine) in preserving potential life became impossible to control, allows countries to freely regulate and even ban after 28 weeks. Next (1992) modifying the "trimester framework," which allows the state to regulate abortion in a way that does not pose a "" to the right of the mother to have an abortion at any point prior to viability; on account of technological developments between 1973 and 1992, survival itself is legally separated from the hardline 28 weeks, leaving the point where "undue burden" is a permissible variable depending on the technology of the time and the judgment of the state legislature.
In 2002, the US government enacted. While the fetus might be feasible or not feasible in the uterus, this law provides the legal definition of personal human life when it is not in the uterus. It defines "born alive" as "complete expulsion or extraction from its or mother of the member, at any stage of development, who after the expulsion or extraction such as breathing or has a heart beating, pulsation of the umbilical cord, or movements that surely voluntary muscles "and determined that all of this is the action of human life. While the implications of this law for defining survival in treatment can not be fully explored, in practice physicians and nurses advised not realize these people with a gestational age of 22 weeks or less, below 400 g weight, with anencephaly, or with a confirmed diagnosis of trisomy 13 or 18.
Forty-three states have laws that restrict post-viability abortions. Some allow doctors to decide for itself whether the fetus is viable. Some require doctors to perform tests to prove the fetus is pre-viable and requires some physicians to validate the findings. Procedure (BEI) becomes the focal point in the abortion debate, based on the belief that it is used mainly post-viability. BEI was made illegal in most circumstances to 2003, in which the US Supreme Court upheld in the case.
Limit survival is where / has a 50% chance of long term survival outside the womb. With support, eligibility limit in developed countries has been declining since 50 years ago.
Currently, the limit of viability is considered about 24 weeks, although the incidence of major defects remain high at this time. Neo-natologists generally will not provide intensive care at 23 weeks, but will be of 26 weeks.
Different jurisdictions have different policies regarding the resuscitation of very preterm newborns, which may be based on various factors such as gestational age, weight and medical presentations infant, wishes of parents and medical practitioners. High risk of severe disability of extremely premature infants or death despite medical efforts led to an ethical debate on and, but also about the sanctity of life as seen in the various religious doctrines.
In 2006, for the survival of premature birth are considered (born on May 20, 1987, Canada, at 21 weeks and 5 days gestation), and Amillia Taylor (IVF pregnancy, was born on October 24, 2006 in ,, at 21 weeks and 6 days of gestation). The second child was born just under 20 weeks from conception (or 22 weeks gestation). At birth, he is 9 inches (22.86 cm) long and weighs 10 ounces (283 grams). He suffered and problems, together with. He was dismissed from Baptist Children's Hospital on February 20, 2007. In 2013, Taylor was in kindergarten and at the small end of normal with some developmental delays.
A, also known as preterm birth, defined as babies born alive before 37 weeks of gestation is complete. There are three types of preterm birth: very preterm (less than 28 weeks), very preterm (28-32 weeks) and medium to late preterm (32-37 weeks).
There are several factors that affect the baby's chance of survival. Two important factors are age and weight. Baby (number of completed weeks of gestation) at birth and birth weight (also the growing size) influence whether the baby will survive. Another major factor is gender: male babies were slightly underdone [] and have a slightly higher risk of death than a baby girl [].
Some types of health problems also affect the viability of the fetus. For example, respiratory problems, congenital abnormalities or malformations, and the presence of other serious illnesses, especially infections, threatening the survival of the newborn.
Other factors may affect survival by changing the degree of maturation of organs or by changing the oxygen supply to the developing fetus.
maternal health plays an important role in the survival of children. Diabetes in the mother, if not controlled properly, slowing the maturation of the organ; The infants of mothers have a higher mortality rate. Severe high blood pressure before the 8th month of pregnancy can cause changes in the placenta, decreased transfer of nutrients and / or oxygen to the fetus and cause problems before and after birth.
before 24 weeks of gestation with loss of amniotic fluid substantially reduces the possibility of infant survival, even if the baby was born shortly thereafter.
The quality of facility-whether deals neonatal hospital critical care services, whether it is a level I pediatricc trauma care facilities, availability of corticosteroids and other drugs in the facilities, experience and the number of doctors and nurses in neonatology and obstetrics and providers have limited but still significant impact on the viability of the fetus. Facilities that have obstetric services and emergency rooms and operating facilities, even if it is smaller, it can be used in areas where a higher service is not available to stabilize the mother and fetus or neonate until they can be transferred to the appropriate facility.
 Definition of Premature Birth - INHA - Irish Neonatal Health Alliance
Definition of Premature Birth - INHA - Irish Neonatal Health Alliance Fetal viability - Wikipedia
Fetal viability - Wikipedia 24 week premature baby's story of survival At 24 weeks - Kidspot
24 week premature baby's story of survival At 24 weeks - Kidspot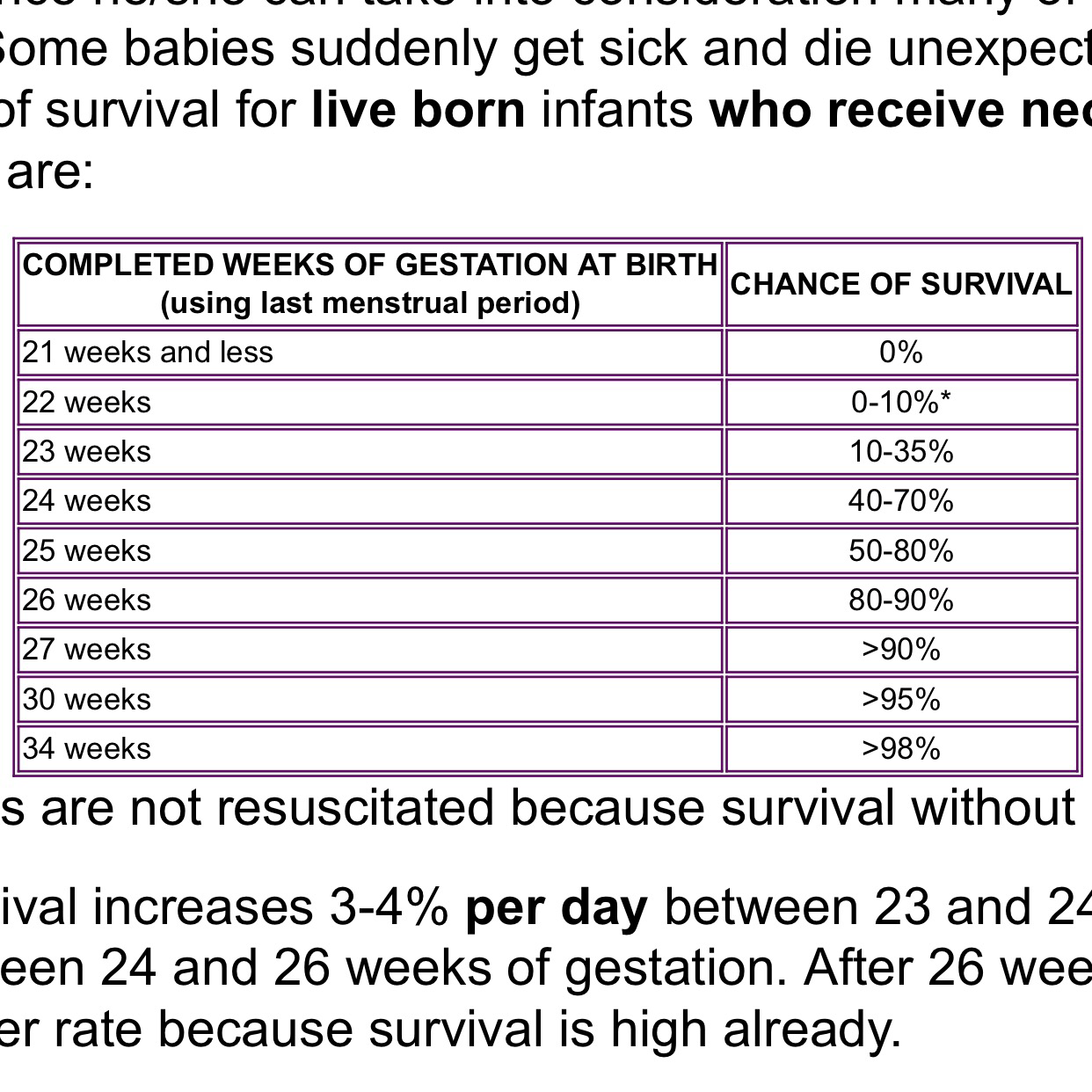 24 weeks! Viability week!!!!! – Growing Baby K
24 weeks! Viability week!!!!! – Growing Baby K Premature babies: How 24 week-old babies are now able to survive ...
Premature babies: How 24 week-old babies are now able to survive ... Should newborns at 22 or 23 weeks' gestational age be aggressively ...
Should newborns at 22 or 23 weeks' gestational age be aggressively ... Should newborns at 22 or 23 weeks' gestational age be aggressively ...
Should newborns at 22 or 23 weeks' gestational age be aggressively ... 4 babies who prove babies born before 24 weeks can survive
4 babies who prove babies born before 24 weeks can survive The Economist explains - The limit of viability | The Economist ...
The Economist explains - The limit of viability | The Economist ... 24 week premature baby's story of survival At 24 weeks - Kidspot
24 week premature baby's story of survival At 24 weeks - Kidspot 23 Week Viability Milestone! — The Bump
23 Week Viability Milestone! — The Bump 4 babies who prove babies born before 24 weeks can survive
4 babies who prove babies born before 24 weeks can survive Premature Twins Born at 24 Weeks Were Given No Chance of Surviving ...
Premature Twins Born at 24 Weeks Were Given No Chance of Surviving ... 24 week premature baby's story of survival At 24 weeks - Kidspot
24 week premature baby's story of survival At 24 weeks - Kidspot The tiniest babies, the toughest decisions | Micro preemie, Nicu ...
The tiniest babies, the toughest decisions | Micro preemie, Nicu ... Photos show incredible transformation of premature baby born at 23 ...
Photos show incredible transformation of premature baby born at 23 ... Britain's smallest baby born at 23 weeks and 4 days weighed just ...
Britain's smallest baby born at 23 weeks and 4 days weighed just ... Can a baby survive pre-term labor at 27 weeks , weighting almost 2 ...
Can a baby survive pre-term labor at 27 weeks , weighting almost 2 ... Born before 22 weeks, 'most premature' baby is now thriving - CNN
Born before 22 weeks, 'most premature' baby is now thriving - CNN Premature baby | Pregnancy Birth and Baby
Premature baby | Pregnancy Birth and Baby What's The Earliest A Baby Can Be Born And Survive? | BellyBelly
What's The Earliest A Baby Can Be Born And Survive? | BellyBelly Nathan was born at 23 weeks. If I'd known then what I do now, I'd ...
Nathan was born at 23 weeks. If I'd known then what I do now, I'd ... Preterm birth - Wikipedia
Preterm birth - Wikipedia:max_bytes(150000):strip_icc()/BeFunky_Jax.jpg-56a7666e3df78cf772959357.jpg) Premature Birth Facts and Statistics
Premature Birth Facts and Statistics Peyton's Preterm Birth
Peyton's Preterm Birth Pregnancy in doctor who, can i get pregnant at 49 naturally, 24 ...
Pregnancy in doctor who, can i get pregnant at 49 naturally, 24 ... Finley had 10% chance of survival at 24 weeks birth. Miraculously ...
Finley had 10% chance of survival at 24 weeks birth. Miraculously ... UK's tiniest baby who weighed the same as 12oz Coke can and had ...
UK's tiniest baby who weighed the same as 12oz Coke can and had ... Miracle Baby Born at 22 Weeks and Given a 2% Chance of Survival ...
Miracle Baby Born at 22 Weeks and Given a 2% Chance of Survival ... Utah baby born at 24 weeks with 'zero percent' chance of survival ...
Utah baby born at 24 weeks with 'zero percent' chance of survival ... 24 Weeks Pregnant | Your Pregnancy Week-by-Week | Bounty
24 Weeks Pregnant | Your Pregnancy Week-by-Week | Bounty Finding That Babies Born at 22 Weeks Can Survive Could Change ...
Finding That Babies Born at 22 Weeks Can Survive Could Change ... Lung Problems in the Premature Baby
Lung Problems in the Premature Baby Baby born at 24 weeks weighing 1lb 7oz survives after docs 'admit ...
Baby born at 24 weeks weighing 1lb 7oz survives after docs 'admit ... Meet the miracle baby boy born at 22 WEEKS | Daily Mail Online
Meet the miracle baby boy born at 22 WEEKS | Daily Mail Online Utah baby born at 24 weeks with 'zero percent' chance of survival ...
Utah baby born at 24 weeks with 'zero percent' chance of survival ... Photos show incredible transformation of premature baby born at 23 ...
Photos show incredible transformation of premature baby born at 23 ... Pregnant mum whose baby has no chance of survival outside womb ...
Pregnant mum whose baby has no chance of survival outside womb ... Premature birth statistics | Tommy's
Premature birth statistics | Tommy's Key questions that arise when a pregnant woman is on life support
Key questions that arise when a pregnant woman is on life support Baby born 14 weeks prematurely becomes one of the smallest to ...
Baby born 14 weeks prematurely becomes one of the smallest to ... PDF) Should we Re-Define Age of Fetal Viability in Nigeria? A Case ...
PDF) Should we Re-Define Age of Fetal Viability in Nigeria? A Case .../rbhc_33-56a6291e5f9b58b7d0e035e6.jpg) Premature Birth and Survival Statistics
Premature Birth and Survival Statistics Premature Birth: Chance of Baby Survival at Weeks 24-37+ ...
Premature Birth: Chance of Baby Survival at Weeks 24-37+ ... 4 babies who prove babies born before 24 weeks can survive
4 babies who prove babies born before 24 weeks can survive Premature rupture of membranes with oligo- or anhydramnios before ...
Premature rupture of membranes with oligo- or anhydramnios before ... Baby girl born at 24 weeks with hands the size of a penny thriving ...
Baby girl born at 24 weeks with hands the size of a penny thriving ... Survival Rates by Gestational Age
Survival Rates by Gestational Age Premature birth & premature babies | Raising Children Network
Premature birth & premature babies | Raising Children Network Survival at Just 25 Weeks - UnityPoint Health
Survival at Just 25 Weeks - UnityPoint Health The Limits of Viability: How Small Is Too Small? - ppt video ...
The Limits of Viability: How Small Is Too Small? - ppt video ... Born before 22 weeks, 'most premature' baby is now thriving - CNN
Born before 22 weeks, 'most premature' baby is now thriving - CNN
Posting Komentar
Posting Komentar